Understanding Major Depressive Disorder: Insights and Approaches
Written on
Introduction to Major Depressive Disorder
Major Depressive Disorder (MDD), commonly referred to as depression, is a prevalent mental health issue. It is characterized by persistent feelings of sadness or a noticeable disinterest in activities that were once enjoyable. Unlike typical mood fluctuations associated with daily life, depression can significantly impact various facets of an individual's life, including personal relationships and professional responsibilities.
This disorder can affect anyone, though those who have experienced trauma, significant losses, or prolonged stress are particularly vulnerable. Statistically, women are more frequently diagnosed with depression than men. MDD is marked by one or more episodes of depression lasting for at least two weeks, which entail considerable alterations in mood, cognition, and physical well-being. The DSM-5, published in 2013, sets forth the criteria for diagnosing MDD.
Post-puberty, the prevalence of MDD in women is approximately double that of men, affecting around 6% of adults globally each year. Among various health conditions, MDD ranks as the second leading cause of long-term disability. It is also associated with a heightened risk for developing chronic illnesses, including diabetes, heart disease, and strokes, which exacerbates its overall impact. Tragically, MDD is a significant risk factor for suicide; nearly 800,000 individuals take their lives globally each year, many during depressive episodes. Those suffering from MDD are nearly 20 times more likely to die by suicide compared to the general population.
The genetic influence on MDD is estimated to be between 30% and 40%, with family studies indicating a higher heritability than estimates derived from SNP-based genome-wide association studies.

The Course and Public Health Implications of MDD
The progression of Major Depressive Disorder (MDD) can vary widely, with significant differences in recovery and chronicity. Research indicates that the average duration of a depressive episode can span from 13 to 30 weeks, with approximately 70-90% of individuals recovering within a year. However, in clinical settings, the prognosis may be less optimistic: only 25% of patients achieve remission within six months, and over half remain depressed after two years. Even after achieving remission, many continue to experience residual symptoms and functional difficulties. The risk of relapse is substantial, with around 80% of individuals facing one or more recurrences post-remission.
The trajectory of MDD in adults tends to worsen with age, but the most significant factors affecting its course are clinical characteristics. More severe symptoms, the presence of other psychiatric conditions, and a history of childhood trauma are strong indicators of a less favorable outcome.
According to the Global Burden of Disease Consortium in 2013, MDD was the second-largest contributor to global health burdens, as measured in disability-adjusted life years, across both developed and developing nations. The repercussions of MDD extend to physical health as well, with extensive studies showing that it elevates the risk for various conditions such as diabetes, heart disease, strokes, hypertension, obesity, cancer, cognitive decline, and Alzheimer's disease. MDD increases the mortality risk by 60-80%, contributing to around 10% of all-cause mortality. If MDD could be eradicated, mortality rates could potentially decrease by 10%.
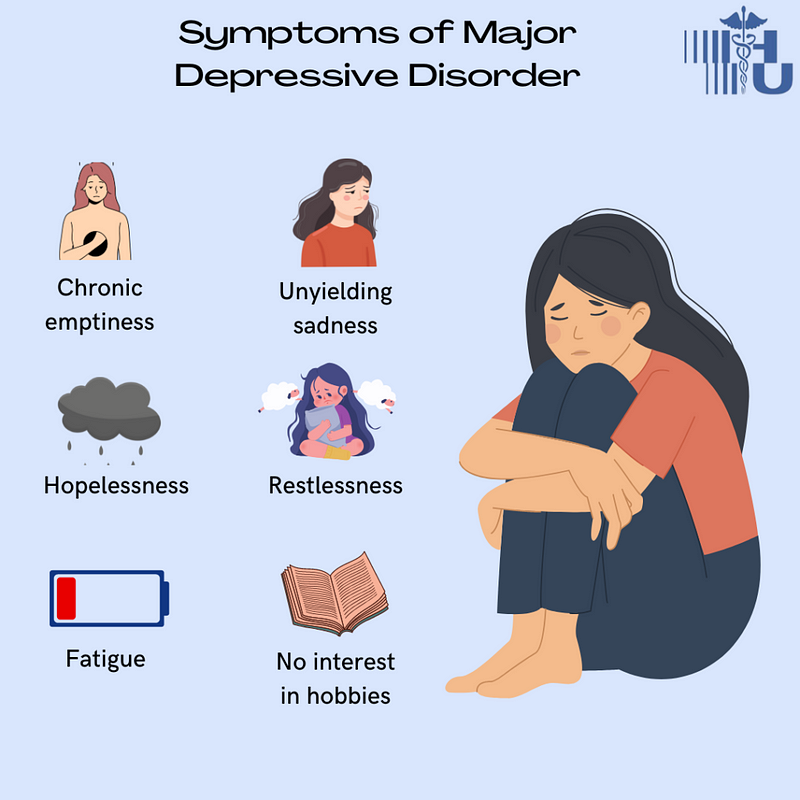
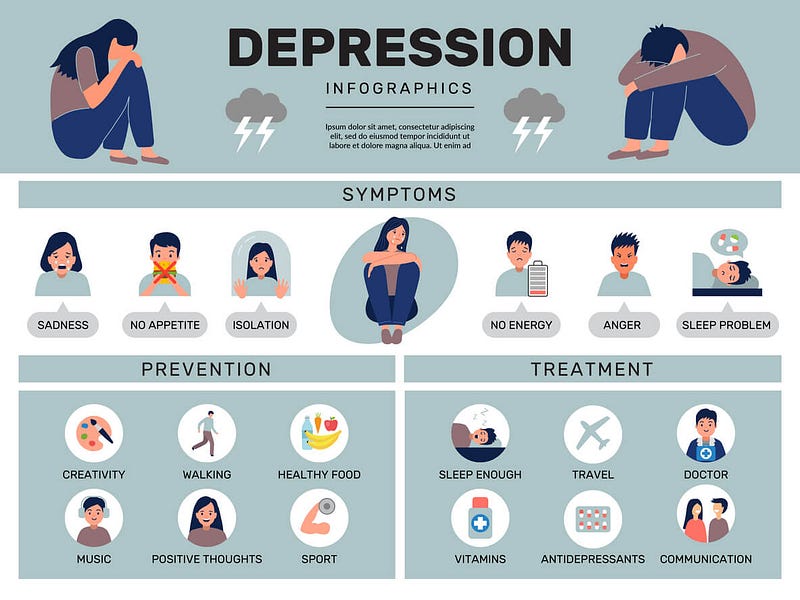
Symptoms of MDD
Individuals with MDD may experience a range of symptoms, which can include:
- Difficulty concentrating
- Overwhelming feelings of guilt or low self-esteem
- Pessimism about the future
- Suicidal thoughts
- Sleep disturbances
- Changes in appetite or weight
- Persistent fatigue or low energy
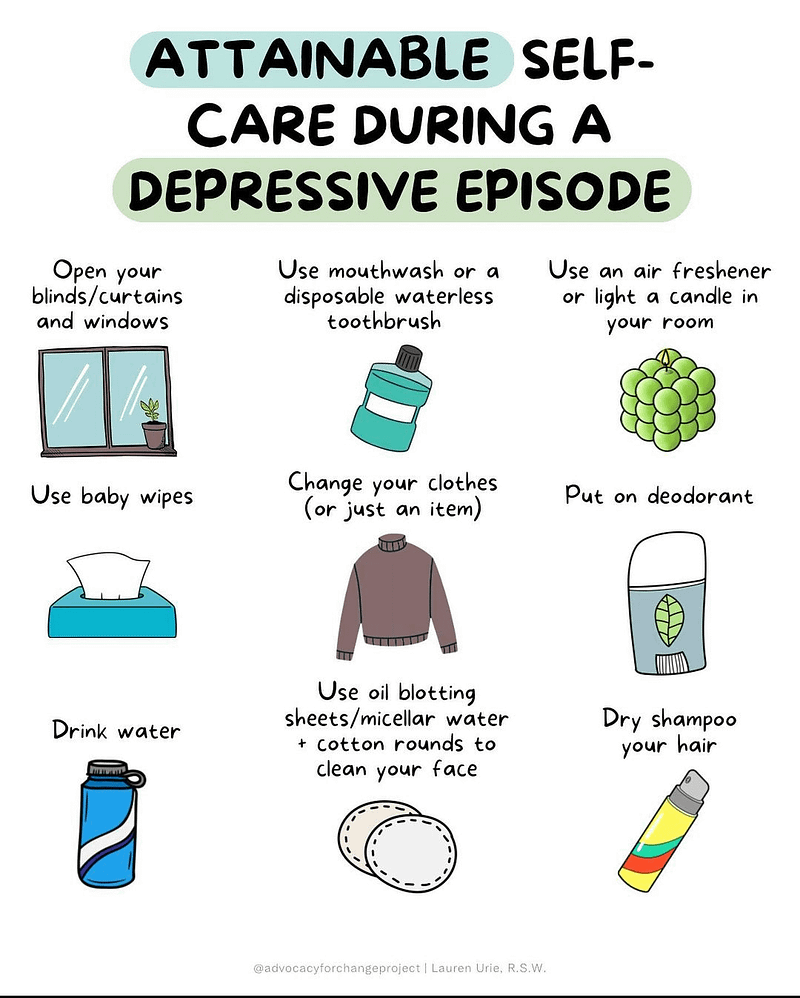
The Role of Self-Care
Engaging in self-care practices can significantly aid in managing depression symptoms and enhancing overall well-being. Here are some strategies to consider:
- Continue participating in activities that once brought joy
- Maintain connections with friends and family
- Incorporate regular physical activity into your routine, even if it's just a short walk
- Strive to keep consistent eating and sleeping patterns
- Limit or eliminate alcohol consumption and avoid illicit substances that may worsen depression
- Share your feelings with someone you trust
- Seek professional help when needed
If you are experiencing suicidal thoughts, remember:
- You are not alone; many others have faced similar challenges and found support.
- Open up to someone you trust about your feelings.
- Consult a healthcare professional, such as a doctor or counselor.
Medical Treatment Options
Psychological therapies are often the first line of treatment for depression, and they can be paired with antidepressant medications in cases of moderate to severe depression. Generally, medications are not necessary for mild depression.
Therapeutic interventions can impart new perspectives on thinking, coping mechanisms, and interpersonal relationships. These may include talk therapy with qualified professionals or supervised lay therapists, and sessions can be conducted in person or online. Additionally, psychological treatments can be accessed through self-help materials, websites, and applications.
Some effective psychological treatments for depression include:
- Behavioral activation
- Cognitive behavioral therapy
- Interpersonal psychotherapy
- Problem-solving therapy
Understanding Major Depressive Disorder: Video Resources
The following video provides an overview of Major Depressive Disorder, discussing its characteristics and treatment options.
The second video further elaborates on Major Depressive Disorder, offering insights into its impact and management.